49 year old obese male, with PMHx of HTN, DM2, asthma, presents to the clinic with c/o lower back pain x 4 weeks. Pt claims the back pain started when he was driving home from New jersey 4 weeks ago. He has had two other visits in the past 4 weeks for the same compliant. Pain is aching, localized to the lower lumbar region, intermittent, 5/10 in intensity, and does not radiate. Patient states the pain is better when he is lying down or walking, but worse with sitting. Pt has been taking ibuprofen 600 mg as needed with minimal relief. Pt states he was sent out for X-ray of the back a week ago which showed no abnormalities. Pt is still concerned and wants to be sent out for an MRI. Denies any family hx of cancers, trauma/fall, saddle anesthesia, numbness/tingling, fevers, weight loss, CP, SOB, abdominal pain, bowel or urinary incontinence, or heavy weight lifting.
I searched for and article that could help me develop the best plan for this patient.
Low Back Pain
Golob, A. L., & Wipf, J. E. (2014). Low Back Pain. Medical Clinics of North America, 98(3), 405–428. doi:10.1016/j.mcna.2014.01.003
This is a 2014 review article published by Medical Clinics of North America journal. This journal provides concise and comprehensive coverage of the issues that providers commonly encounter.
Articles Key Points:
- Physical exam plays a huge role in back pain.
- Main focus of physical exam is to evaluate the patient for any systemic or pathological cause that may be contributing to back pain.
- Most back pain is non-specific and will resolve with or without treatment.
- The approach to back pain is tailored to preventing disability and preserving function.
- Patients with acute nonspecific low back pain should be given general self-care advice. Advise the patient to return to usual activity and the avoid of prolonged bed rest of more than 3 days.
- Short term analgesia can be prescribed to help alleviate short term pain.
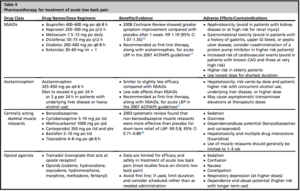
- Classes of medications shown to provide some pain relief for low back pain, include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, skeletal muscle relaxants, tramadol, and opioids.
- The 2007 joint guidelines from the ACP and American Pain Society recommend either NSAIDs or acetaminophen as first-line analgesic agents for the treatment of low back pain.
- Pharmacotherapy not recommended, due to weak supporting evidence include, systemic glucocorticoids, lidocaine patches, anticonvulsants, or antidepressants in the treatment of acute low back pain.
- There are no high-quality studies that support that nonpharmacologic therapies are superior to self-care advice in the treatment of acute low back pain.
- Non-pharmacologic therapies may benefit patients who are considered to be at higher risk for prolonged pain and disability.
Treatments for chronic back pain:
Imaging is not warranted unless patient has:
- No improvement with initial treatment for up to 4-6 weeks
- Evidence of systemic causes, infection, fracture, malignancy, or neurological deficits.
Emergent imaging in patients with signs of cauda equina or sever progressive neurological decline.

Article provided an excellent algorithm that could be used to help guide the evaluation of low back pain. (See below)


Surgical outcomes may be superior to nonsurgical management in the short term. Long term follow-up shows no differences in outcome.
Surgical evaluation is recommended for patients with:
- severe or progressive motor weakness
- evidence of cauda equina syndrome
Elective surgery for patients with:
- Radiculopathy and spinal stenosis, which is unresponsive to nonsurgical treatments, and is associated with chronic disabling symptoms


