Home » News
Category Archives: News
Cover Letter
Dear (insert name)
I am a Physician Assistant student graduating in December 2019 from CUNY York College, and I am very interested in being hired for the Physician Assistant opening in your ______ DEPT.
During my life I have always found joy in providing care to others, which is why I chose to become a Physician Assistant. As a Physician Assistant, I hope to be empathetic with my patients and be able to provide quality compassionate care to them. I believe in order to be good providers we must also understand the importance of being culturally aware when treating our patients. My volunteer experience at New York Hospital of Queens (ED and L&D) consisted of a very diverse, culturally rich population, giving me the opportunity to become a more culturally informed individual.
As a Medical assistant I develop my EMR skills, along with adopting good interviewing and procedural skills. As I made my transition to site manager of the Urgent care, I was able to increase my interpersonal skills, and time management skills. Since providers are constantly on the frontline of patient care, it is important to work well under pressure, and stay calm and collected when confronted with stress full situations. Being in charge of patient satisfaction during my role as manager allowed me to become well prepared in handling stressful situations, a skill that can be very valuable to me as a provider. Furthermore, the knowledge I attained during my clinical rotations has given me a solid foundation for practice and has helped me adopt great bedside manners. Additionally, I am confident my ability to speak multiple languages (Pashto, Urdu, and English) can help me overcome the language barrier during many of my future patient interactions. My clinical and personal experiences have shaped me into a more patient, empathetic, and culturally competent provider.
My ability to work well with team members, good work ethic, strong communication skills, and fluency in multiple languages, makes me a good candidate for this position. I strongly believe I can be a valuable addition to your team, and I hope you will consider me for this position. Thank you for your time, and I hope to hear from you soon.
Best,
Toor Noori
Article summary
49 year old obese male, with PMHx of HTN, DM2, asthma, presents to the clinic with c/o lower back pain x 4 weeks. Pt claims the back pain started when he was driving home from New jersey 4 weeks ago. He has had two other visits in the past 4 weeks for the same compliant. Pain is aching, localized to the lower lumbar region, intermittent, 5/10 in intensity, and does not radiate. Patient states the pain is better when he is lying down or walking, but worse with sitting. Pt has been taking ibuprofen 600 mg as needed with minimal relief. Pt states he was sent out for X-ray of the back a week ago which showed no abnormalities. Pt is still concerned and wants to be sent out for an MRI. Denies any family hx of cancers, trauma/fall, saddle anesthesia, numbness/tingling, fevers, weight loss, CP, SOB, abdominal pain, bowel or urinary incontinence, or heavy weight lifting.
I searched for and article that could help me develop the best plan for this patient.
Low Back Pain
Golob, A. L., & Wipf, J. E. (2014). Low Back Pain. Medical Clinics of North America, 98(3), 405–428. doi:10.1016/j.mcna.2014.01.003
This is a 2014 review article published by Medical Clinics of North America journal.This journal provides concise and comprehensive coverage of the issues that providers commonly encounter.
Articles Key Points:
- Physical exam plays a huge role in back pain.
- Main focus of physical exam is to evaluate the patient for any systemic or pathological cause that may be contributing to back pain.
- Most back pain is non-specific and will resolve with or without treatment.
- The approach to back pain is tailored to preventing disability and preserving function.
- Patients with acute nonspecific low back pain should be given general self-care advice. Advise the patient to return to usual activity and the avoid of prolonged bed rest of more than 3 days.
- Short term analgesia can be prescribed to help alleviate short term pain.
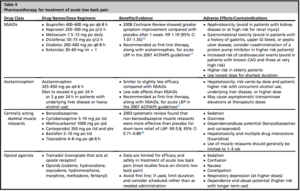
- Classes of medications shown to provide some pain relief for low back pain, include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, skeletal muscle relaxants, tramadol, and opioids.
- The 2007 joint guidelines from the ACP and American Pain Society recommend either NSAIDs or acetaminophen as first-line analgesic agents for the treatment of low back pain.
- Pharmacotherapy not recommended, due to weak supporting evidence include, systemic glucocorticoids, lidocaine patches, anticonvulsants, or antidepressants in the treatment of acute low back pain.
- There are no high-quality studies that support that nonpharmacologic therapies are superior to self-care advice in the treatment of acute low back pain.
- Non-pharmacologic therapies may benefit patients who are considered to be at higher risk for prolonged pain and disability.
Treatments for chronic back pain:
Imaging is not warranted unless patient has:
- No improvement with initial treatment for up to 4-6 weeks
- Evidence of systemic causes, infection, fracture, malignancy, or neurological deficits.
Emergent imaging in patients with signs of cauda equina or severe progressive neurological decline.

Article provided an excellent algorithm that could be used to help guide the evaluation of low back pain. (See below)


Surgical outcomes may be superior to nonsurgical management in the short term. Long term follow-up shows no differences in outcome.
Surgical evaluation is recommended for patients with:
- severe or progressive motor weakness
- evidence of cauda equina syndrome
Elective surgery for patients with:
- Radiculopathy and spinal stenosis, which is unresponsive to nonsurgical treatments, and is associated with chronic disabling symptoms
Reflection on evaluation FM
For our first FM site evaluation we came prepared with 2 H&Ps, and 5 pharm cards. We first went over the pharm cards after which I discussed my cases. The first patient I presented was a 56 y/o M with PMHx of OA of the knee, Diabetes, HTN, and HLD. He presents to the clinic with c/o pain on the hallux of his right foot x 3 months. Pt’s physical exam reveals a 2 cm lump, and skin thickness on the lateral aspect on the hallux. There was pain and tenderness on palpation. Symptoms and PE were consistent with hallux bunion. This case was very straightforward, and the plan was to refer to podiatry for further evaluation. The second a patient I presented came in with c/o diffuse abdominal pain x 1 day. Pain was constant, crampy pain, 8/10 in intensity, did not radiate and was associated with nausea, and two episodes of diarrhea followed by constipation and absence of flatulence x 1 day. This patient history and presentation (hypoactive bowl sounds, distended belly) caused suspicion of SBO. We sent her the patient to the ER and advised the patient not to eat anything until she was further evaluated there. We followed up with her the next day to learn she was discharged with no abnormal findings during her ED workup. Professor Mohammad explained that our differential was very valid since he too felt the patient sounded as if she may have an obstruction. He also agreed with our plan and explained how it was important to follow up with our patients in family care something he probably did less of in emergency medicine.
For the second evaluation we once again started off with 5 pharm cards, and I presented one case, along with an article to support my plan for the patient. This patient presented to the clinic with c/o lower back pain x 4 weeks. Pain started when he was driving home from his son’s home in New jersey 4 weeks ago. He has had two other visits to our clinic in the past 4 weeks for the same compliant. Pain was aching, localized to the lower lumbar region, intermittent, 5/10 in intensity, and dis not radiate. Pain was better when he is lying down or walking, but worse with sitting. Pt had been taking ibuprofen 600 mg as needed with minimal relief. Lumbar X-ray, CRP, CBC, was done last visit and showed no abnormalities. Pt was very concerned and wanted to be sent out for an MRI. He denied any family hx of cancers, trauma/fall, saddle anesthesia, numbness/tingling, fevers, weight loss, CP, SOB, abdominal pain, bowel or urinary incontinence, or heavy weight lifting. On exam he was in NAD, straight leg raise was neg, no scoliosis/lordosis/kyphosis, sensory and muscle strength was intact, and no neurological deficits. There was no para-vertebral tenderness or tenderness on palpation of the spinal processes. I found a 2014 review article which helped me formulate the best possible plan for him. It also helped to determine if an MRI was indicated in his case.
The article provided a guide on how to manage patients with acute lower back pain. It explained that imaging is not indicated in patients with no evidence of systemic causes, infection, fracture, malignancy, or neurological deficits. The article also provided other possible pharmacological and non-pharmacological treatment options for this patient.
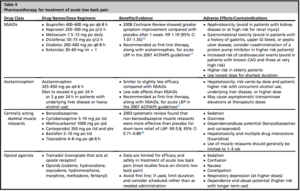
The patient was currently only taking NSAIDS as needed, so we decided to add on a muscle relaxant (cyclobenzaprine 5 mg TID) to his current treatment plan and scheduled him for follow within 2 weeks. We advised him to continue on with his usual daily activities as tolerated and refrain from excessive bed rest. The article points out that most non-specific lower back pain usually resolves on its own. I really liked that Professor Mohammed was interested to learn how to manage back pain in the put patient setting. He explained he didn’t have much experience with outpatient back pain and he would have done an MRI on the patient in the ED. Especially since it was his third visit. After the evaluation was over, I realized how much I had learned about back pain because of this article. I learned that having us use an article for a case presentation has allowed us to master how to manage certain conditions, in this case back pain. This is helping us become more competent providers, by forming a good habit for us to carry on with us to our practices in the future. I will continue to use Evidence based medicine, to help me with my approach to patients and formulation of their treatment plans.
After the presentation of my article Professor Mohammed asked us to share our experience from our rotations. He then explored which were potential specialties we may consider after graduation. He also provided us with excellent advice on important factors to consider when accepting a job position. He then shared his personal experiences with us and gave us information on potential jobs opportunities. I was so grateful to him for taking the extra time to guide us in the right direction.
Site reflection FM
I had the pleasure of doing my Family Medicine rotation with Dr. Diaro as my preceptor. The facility was called Amazing Medical Clinic (AMZ), and it was nothing short of amazing. The clinic really lived up to its name. This office has an excellent team which consisted of the kindest and most lovable human beings you will ever meet. This wonderful team was made up of 5 individuals named Tola, Sandy, Joanne, Bookie, and Dr. Diaro. They easily welcomed me into their team and provided me with both emotional and technical support needed to practice competently. One thing I really admired about the people at the rotation was that they started off each day with a prayer. They prayed for the health of their patients, and for strength to provide proper care to anyone who walked into their office. This showed me that people at this office were very dedicated to caring for their patient’s heath. As a temporary member of the team I allowed to be a part of this prayer each morning, which I am so very grateful for.
Family Medicine was different from my other rotations, in the sense that it allowed me to spend a longer amount of time with the patient during each encounter. This was something I really enjoyed, because it gave me time to get to know my patient very well, something that was not as prevalent at other rotations. I enhanced my skills at performing focused exams, diabetic foot exams, and procedures (ex: blood draws, EKG’s, spirometry, injections, and PPD placements). I really liked that Dr. Diaro was very up to date with new guidelines and recommendations for the common conditions we would encounter. She was very good at practicing Evidence based Medicine, and made frequent references to new research. This taught me that no matter how much experience you may have you should always stay up to date with changing guidelines.
Something else that I really appreciated about this rotation was that, Dr. Diaro took the time each day to stop and thank the staff and myself. She would acknowledge my hard work, and complement me on my HPI’s, assessment/ treatment plans, and procedural skills. She agreed with my plans most of the time, but when she didn’t she never made me feel as if I was wrong. Instead she would explain why she would do something different for the patient, and then she would have me look it up, and come back to let her know if I agreed. This made me feel as if we were working as a team to treat the patient and I was a part of the decision making. I also appreciated that she referred to the patients that I saw as “your patient”, this allowed me to feel more autonomous and help build my confidence as a provider. She never had an issue sharing the credit with me or any other member of the staff, which I feel is an important factor in forming a healthy relationship with the individuals we work with. We at the office all knew she was far more intelligent than we were, but she never allowed us to feel it. This made everyone want to work their hardest and provided a healthy environment for both staff members and patients. From this I learned that when a Physician, PAs, and staff members have a strong relationship, it in turn reflects on the care provided to patients of that practice.
This rotation taught me how to formulate plans for patients with a large variety of complaints, provide preventative care, manage chronic care patients, perform employment/ immigration/DOT physicals, but more importantly it taught me how to work in a team, interact with patients, build rapport, and personalized my encounters with my patients. These are skill that I can take with me to any practice I choose, whether it be a specialty, emergency medicine, or primary care.

