For our first FM site evaluation we came prepared with 2 H&Ps, and 5 pharm cards. We first went over the pharm cards after which I discussed my cases. The first patient I presented was a 56 y/o M with PMHx of OA of the knee, Diabetes, HTN, and HLD. He presents to the clinic with c/o pain on the hallux of his right foot x 3 months. Pt’s physical exam reveals a 2 cm lump, and skin thickness on the lateral aspect on the hallux. There was pain and tenderness on palpation. Symptoms and PE were consistent with hallux bunion. This case was very straightforward, and the plan was to refer to podiatry for further evaluation. The second a patient I presented came in with c/o diffuse abdominal pain x 1 day. Pain was constant, crampy pain, 8/10 in intensity, did not radiate and was associated with nausea, and two episodes of diarrhea followed by constipation and absence of flatulence x 1 day. This patient history and presentation (hypoactive bowl sounds, distended belly) caused suspicion of SBO. We sent her the patient to the ER and advised the patient not to eat anything until she was further evaluated there. We followed up with her the next day to learn she was discharged with no abnormal findings during her ED workup. Professor Mohammad explained that our differential was very valid since he too felt the patient sounded as if she may have an obstruction. He also agreed with our plan and explained how it was important to follow up with our patients in family care something he probably did less of in emergency medicine.
For the second evaluation we once again started off with 5 pharm cards, and I presented one case, along with an article to support my plan for the patient. This patient presented to the clinic with c/o lower back pain x 4 weeks. Pain started when he was driving home from his son’s home in New jersey 4 weeks ago. He has had two other visits to our clinic in the past 4 weeks for the same compliant. Pain was aching, localized to the lower lumbar region, intermittent, 5/10 in intensity, and dis not radiate. Pain was better when he is lying down or walking, but worse with sitting. Pt had been taking ibuprofen 600 mg as needed with minimal relief. Lumbar X-ray, CRP, CBC, was done last visit and showed no abnormalities. Pt was very concerned and wanted to be sent out for an MRI. He denied any family hx of cancers, trauma/fall, saddle anesthesia, numbness/tingling, fevers, weight loss, CP, SOB, abdominal pain, bowel or urinary incontinence, or heavy weight lifting. On exam he was in NAD, straight leg raise was neg, no scoliosis/lordosis/kyphosis, sensory and muscle strength was intact, and no neurological deficits. There was no para-vertebral tenderness or tenderness on palpation of the spinal processes. I found a 2014 review article which helped me formulate the best possible plan for him. It also helped to determine if an MRI was indicated in his case.
The article provided a guide on how to manage patients with acute lower back pain. It explained that imaging is not indicated in patients with no evidence of systemic causes, infection, fracture, malignancy, or neurological deficits. The article also provided other possible pharmacological and non-pharmacological treatment options for this patient.
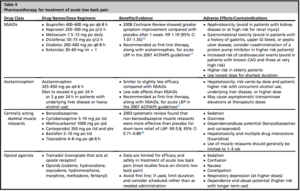
The patient was currently only taking NSAIDS as needed, so we decided to add on a muscle relaxant (cyclobenzaprine 5 mg TID) to his current treatment plan and scheduled him for follow within 2 weeks. We advised him to continue on with his usual daily activities as tolerated and refrain from excessive bed rest. The article points out that most non-specific lower back pain usually resolves on its own. I really liked that Professor Mohammed was interested to learn how to manage back pain in the put patient setting. He explained he didn’t have much experience with outpatient back pain and he would have done an MRI on the patient in the ED. Especially since it was his third visit. After the evaluation was over, I realized how much I had learned about back pain because of this article. I learned that having us use an article for a case presentation has allowed us to master how to manage certain conditions, in this case back pain. This is helping us become more competent providers, by forming a good habit for us to carry on with us to our practices in the future. I will continue to use Evidence based medicine, to help me with my approach to patients and formulation of their treatment plans.
After the presentation of my article Professor Mohammed asked us to share our experience from our rotations. He then explored which were potential specialties we may consider after graduation. He also provided us with excellent advice on important factors to consider when accepting a job position. He then shared his personal experiences with us and gave us information on potential jobs opportunities. I was so grateful to him for taking the extra time to guide us in the right direction.


